HST.525: Tumor Microenvironment and Immuno-oncology: A Systems Biology Approach#
Professor: Rakesh K. Jain, PhD
- HST.525: Tumor Microenvironment and Immuno-oncology: A Systems Biology Approach
- Abbreviations
- Definitions
- More reading
- Physical traits of cancer (Nia, Munn, Jain 2020)
- 1. TME I: Angiogenesis and Vascular Function
- 2. TME II: Vascular Normalization and Immunotherapy
- 3. Tumor metabolism
- 4. Drug delivery systems for cancer, COVID, and other diseases
- Questions to pursue
- 5. Tumor Microenvironment III: Extracellular Matrix, Lymphatics, and Metastasis
- 6-1. The lymphatics system in cancer progression
- 6-2. Mechanobiology of tumors and vasculature
- 6-3. Role of translational studies in an era of rapidly evolving strategies for liver cancer treatment
- 7-1. Using chemistry and materials science-based strategies to enhance cancer immunotherapy (Darrell Irvine)
- 7-2. Human T-dependent B cell subsets in tissues and tumors (Shiv Pillai)
- Dai Fukumura, Role of Obesity and Exercise in Cancer
- Yves Boucher, Reprogramming Pancreatic Cancer Tumor Microenvironment to Improve Therapy
- Lei Xu, Targeting the Tumor Microenvironment to Improve Tumor Control and Quality of Life
Abbreviations#
- ASI. angiotensin system inhibitors
- VEGF. vascular endothelial growth factor
- IFP. interstitial fluid pressure
- ICB. immune checkpoint blocker
- TVP. tumor vessel perfusion
- CAF. cancer-associated fibroblast
- YAP. Yes-associated protein
- TAZ. transcriptional co-activator with PDZ-binding motif
Definitions#
- orthotopic. (in medicine) something that occurs in the normal or usual place in the body. For example, transplanting a human breast cancer into the breast region of a mouse as a xenotransplant model is orthotopic.
- stroma. matrix and fibroblasts.
- R0 resection. microscopically margin-negative resection, in which no gross or microscopic tumor remains in the primary tumor bed.
- pre-neoplasia. hyperplasia and dysplasia.
- solid stresses (=residual stresses). the mechanical forces (compressive, tensile, and shear) contained in and transmitted by solid and elastic elements of the ECM and cells.
- matrix metalloproteinases (=MMPs, matrix metallopeptidases, matrixins). enzymes capable of degrading all kinds of extracellular matrix proteins.
- cell glycocalyx. a dense layer of sugars attached to proteins and lipids that cover all cells in the human body.
- microcirculation. the circulation of blood in the smallest blood vessels, the microvessels of the microvasculation present within organ tissues. It includes terminal arterioles, metarterioles, capillaries, and venules.
- pericyte. multi-functional mural cells of the microcirculation that wrap around the endothelial cells that line the capillaries of the body
- stiffness (=rigidity, elastic modulus). resistance of a material to deformation in response to a force applied at a very slow rate (=quasi-statically). Stiffness is an intrinsic material property of the tissue.
More reading#
Physical traits of cancer#
- Myc-driven endogenous cell competition in the early mammalian embryo
- Force-Induced Unfolding of Fibronectin in the Extracellular Matrix of Living Cells
Lecture 1#
- CAFs and TAMs: maestros of the tumour microenvironment
- Vascular regulation of antitumor immunity
- Molecular mechanisms and clinical applications of angiogenesis
- Interstitial Fluid Pressure in Solid Tumors following Hyperthermia: Possible Correlation with Therapeutic Response
- Physical traits of cancer
Physical traits of cancer (Nia, Munn, Jain 2020)#
Solid stress#
- can be <100 Pa in glioblastomas to 10,000 Pa in PDACs
- mechanisms for generating solid stresses in the TME
- increased tissue volume
- caused by cell infiltration, cell proliferation, and matrix deposition; added volume pushes against existing viscoelastic structures (such as vessels)
- concerted displacement of normal tissue
- swelling of existing glycosaminoglycan matrix components such as hyaluronic acid owing to electroosmotic water absorption
- actomyosin-mediated cell contractions
- fibroblasts, immune cells, and cancer cells can all contract matrix elements
- increased tissue volume
- solid stress
- vessel compression
- hypoxia
- less effective delivery of chemo-, radio-, and immunotherapies
- indirect effects on ECM components
- e.g. releasing latent matrix-bound TGF-
- e.g. unfolding of fibronectin
- e.g. enzymatic resistance of collagen fibers
- cell competition
- cancer cells kill normal surrounding cells to expand into new space
- vessel compression
Interstitial fluid pressure#
- from <1 kPa in brain tumors to 5 kPa in renal cell carcinomas; usually 0 in normal tissue
- high IFP
- drives interstitial flow to tumor margin
- extravascular cells exposed to shear stress
- activation of fibroblasts
- modulation of endothelial sprouting
- induction of matrix metalloproteinase (MMP) activity and cell motility
- activation of cancer cell migration and invasion
- extravascular cells exposed to shear stress
- drives interstitial flow to tumor margin
Stiffness (elasticity)#
- from 1 kPa in brain tumors to 70 kPa in cholangiocarcinomas
- high stiffness
- promotes tumor progression (how?)
- promotes invasive phenotype in cancer cells
- induces invasion and metastasis
- enhances immune cell infiltration
- facilitates EMT through TGF-
- promotes stem cell differentiation
- alters growth factor secretion and signaling
- increases angiogenesis and vessel permeability
- causes
- increased deposition and cross-linking of ECM
1. TME I: Angiogenesis and Vascular Function#
Why the TME is important#
- cancer cells are only a part of a tumor
- blood cancers are the easiest to treat
- no microenvironment
- pancreatic cancer is the hardest to treat
- in pancreatic tumors, less than 5% of cells are cancer cells
- host cells
- CAFs (cancer-associated fibroblasts)
- immune cells
- Revolutions in cancer therapy
- genome medicine. target mutations to cure cancer
- less than 5% patients benefit from genomic medicine
- immunotherapy
- still, less than 13% benefit from this therapy
- tumor microenvironment interferes with both techniques
- genome medicine. target mutations to cure cancer
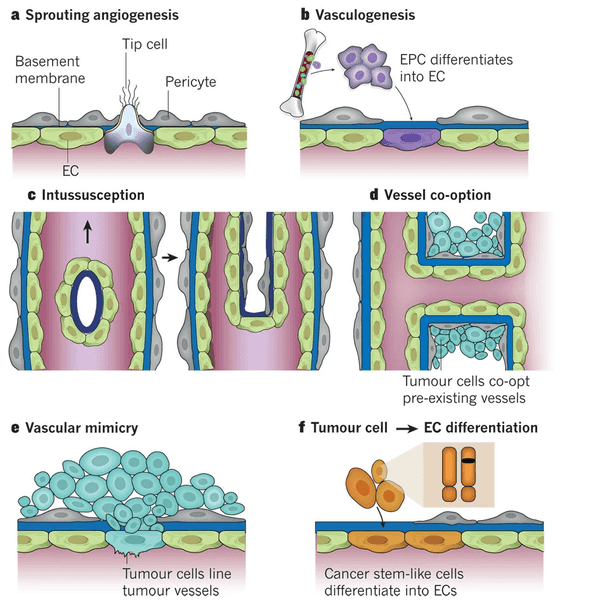
Six modes of neovascularization#
- sprouting angiogenesis
- vasculogenesis
- intussusception
- vessel co-option
- vascular mimicry
- tumor cell EC differentiation
Vascular function#
- Characteristics of TME
- hypoxia
- low pH
- hydrostatic pressure
- microenvironment shapes tumor biology
- whether or not a drug works depends on where the tumor has spread
- Blood flow in tumor vs. normal vessels
- some regions of the tumor have high blood flow; some have none, even if blood vessels are present!
- because the blood vessels are highly irregular, delivering drugs and immune cells requires special care!
- Solid stress and interstitial fluid pressure in tumors
- interstitial fluid pressure is generally 0 in periphery
- in tumors, it can range from 0 to 100+
- Summary
- tumor perfusion rate usually decreases with growth
- impaired blood supply contributes to hypoxia and low pH
- hypoxia and acidosis can induce immunosuppression and treatment resistance (including radiotherapy, which needs oxygen to form oxygen radicals), and fuel tumor progression, invasion and metastasis
Why is tumor blood flow impaired?#
- too much VEGF produced by tumors cause blood vessels to have holes
- solution: don't completely inhibit VEGF, but reduce the concentration to normal levels so we can grow blood vessels to cancers that deliver drugs and oxygen
Where is the hydrostatic pressure in tumors coming from?#
- depletion of cancer cells, stromal cells, collagen I, or HA decreases solid stress
- depletion of cancer cells
- cancer cells can compress vessels
- depletion of stroma
- angiotensor receptor I (AT1) signaling regulates stroma
- use Losartan (blood pressure drug)
- Obesity and cancer
- Obese PDAC patients have poorer prognosis; why?
- obesity induces fibrosis and fuels PDAC progression
- use Losartan again; added nearly 18 months to 5-year survival
- Obese PDAC patients have poorer prognosis; why?
- Losartan and ovarian cancer
- losartan treatment reduces ascites in mice with ovarian cancer by "normalizing" lymphatics
- lymphatics are collapsed too; leaky vessels force fluid to build up in matrix (IFP)
- IFP already increases in pre-neoplasia stages; why?
- evolutionary benefit: prevent immune cells from curbing growth
- causes
- lack of functional lymphatics
- higher vascular permability
- vascular compression
- consequences of elevated IFP
- washes out drugs
- spreads growth-factors (such as VEGF-A, VEGF-C)
- spreads cancer cells to increase metastasis
- can reduce extravasation (giving resistance to treatment)
- IFP already increases in pre-neoplasia stages; why?
2. TME II: Vascular Normalization and Immunotherapy#
- how does TME contribute to immunosuppression?
- increased proliferation of Treg
- convert anti-tumor macrophages to pro-tumor macrophages
- prevent maturation of dendritic cells
- downregulate adhesion molecules
- two strategies to recover blood vessel function
- normalize stroma/ECM
- normalize blood vessels directly
- vascular normalization hypothesis
- preclinical and clinical evidence
- preclinical evidence
- imaging
- measure blood flow (blood flow )
- measure leakiness (leakiness )
- clinical evidence
- glioblastoma
- anti-VEGF blood flow in brain increased 9 month increase in survival
- glioblastoma
- preclinical evidence
- enhancing immunotherapy
- anti-angiogenic therapy (AAT), at the right dose, cause significant increase in immune cell count in tumors
- beyond VEGF: GBM
- why did anti-PD1 alone or with anti-VEGF fail in GBM patients?
- potential mechanisms
- upregulation of angiopoietin 2 (Ang2) (another angiogenic factor)
- anti-PD1 increases cerebral edema
- abundance of regulatory T cells (Tregs) in GBM
- solving 1
- bivalent antibody (called A2V) to block both VEGF and Ang2
- A2V + anti-PD1 antibody = better perfusion
- solving 2
- steroids used to treat edema is immunosuppressive!
- we can reduce edema (reduce leakiness) using ASI
- solving 3
- Tregs are characterized by TF FoxP3
- can we reprogram Tregs into T effector cells?
- yes, with aPD1+aGITR
- avoiding immune toxicity (resistance)
- CD8 memory clls are found only in the tumor draining lymph nodes thus limiting the possibility of irAEs
- potential mechanisms
- why did anti-PD1 alone or with anti-VEGF fail in GBM patients?
- beyond VEGF: ICB
- immune checkpoint blockers can also normalize blood vessels (though not in GBM)
- IFN- might increase TVP
- immune checkpoint blockers can also normalize blood vessels (though not in GBM)
- beyond VEGF: physical aerobic exercise
- exercise can also normalize blood vessels!
- perhaps via CD8 effector T cells
- vessel normalization can decrease metastasis
- potential reason why exercise after treatment reduces recurrence
- exercise can also normalize blood vessels!
- beyond malignant disease
3. Tumor metabolism#
- Warburg hypothesis wrong; the Warburg effect is very real though (observations are always right, hypotheses can be wrong)
- don't fall in love with your own ideas
- not really known why cancer uptakes so much glucose
- metabolism is different from cancer/normal, can take advantage in diagnostic tests
- FDG-PET
- NOT for diagnosis
- for predicting response to therapy
- FLT-PET
- FDG-PET
- no hypoxia selecting for fermentative phenotype (shown in 2016 paper)
- HIF-1 senses oxygen
- more oxygen hydroxylates HIF-1 gets degraded
- the metabolism is probably about making more stuff, not about getting more ATP
- what matters in metabolism is flux
- difference between targeted therapy and old school chemotherapy
- whether you knew the target before or after discovering the drug
- not all cancers rely on the same metabolic pathway
- how do you get differential sensitivity to an "essential" gene? (e.g. thymidine synthase)
- enzyme levels don't mean a reaction is happening! (they are roads, not the cars driving along it)
- cancer cell metabolism is influenced by
- genetic mutation
- lineage
- tissue environment
- metabolism differs between lung cancer cells in culture and lung tumors
- environment can dictate the metabolic phenotype of lung cancer cells
- target essential genes in the right conditions
What is the environment? and metastasis#
- maybe cancer doesn't control its environment, but it has to adapt to it
- seed vs. soil?
- cancers metastasize in very stereotypical anatomical locations
- e.g. prostate goes to bone; no real anatomical explanation
- cancers metastasize in very stereotypical anatomical locations
- cancers prefer to grow in their primary site, even after metastasis
- the tissue environment restricts metastatic tumor growth
- not necessarily true in the brain (brain metastasis; brain environment is different)
- e.g. access to lipids is limited in the brain
- not necessarily true in the brain (brain metastasis; brain environment is different)
- the tissue environment restricts metastatic tumor growth
- metabolism happens on second timescale; cells will not survive long enough to alter gene expression (needs to respond via allostery)
Budget hypothesis#
- oxidation reactions are important to generate biomass
- the currency
- explains fermentation preference in cancer
- need to restore redox balance to make more nucleotides (more oxidized than the food we eat)
- 5-FU depends on pyrimidine salvage; able to treat pyrimidine-salvage dependent cancers (non-small cell lung cancer, pancreatic cancer)
4. Drug delivery systems for cancer, COVID, and other diseases#
- angiogenesis inhibitors
- required surgical fellows and residents to do the animal experiments
- rabbit models
- first delivery, then infusion techniques
- moved to mouse models
- drug delivery itself is interesting
- diabetes insulin delivery
- started a company with four students: Enzytech
- merged with Alkermes; led to controlled drug release systems like Vivetrol
Questions to pursue#
- Post-therapy relapse; why do the cancer cells grow in other locations?
- In general, how have the cancer cells changed?
5. Tumor Microenvironment III: Extracellular Matrix, Lymphatics, and Metastasis#
- EPR (enhanced permeability and retention) should allow for nanomedicine
- however, the nanoparticles are not actually reaching the tumor despite the enhanced permeability
- lymphatics require valves to move fluid
- how to remove nitric oxide to restabilize nitric oxide gradients restore lymphatics
6-1. The lymphatics system in cancer progression#
- optical coherence tomography (OCT)
- metastasis is possible because lymphatics at the edge of the tumor are still functional
- spread to lymph nodes is not a clonal process
- cancer cells that spread to lymph nodes are hypoxic but don't attempt angiogenesis
- blocking angiogenesis doesn't work
- Unsolved questions in cancer biology
- unable to identify which patients are likely to have metastases come from the lymph nodes rather than the tumor itself
- HEV special blood vessels in lymphatics
- pressure can cause HEV remodeling (eliminating the HEVs that allow immune cells into the tumor)
6-2. Mechanobiology of tumors and vasculature#
- mechanobiology: forces as signals
- collective behavior: local rules leading to emergent behavior
- HDAC-1 is involved in flow mechanotransduction
- compression enhances cell-matrix adhesion
- nitric oxide modulates contractions (peristalsis)
6-3. Role of translational studies in an era of rapidly evolving strategies for liver cancer treatment#
- how does antiangiogenic therapy fail in HCC?
- increased fibrosis leads to resistance
- overcoming AAG therapies in HCC by combining it with immunotherapies
- tackling cholangiocarcinoma (bile duct cancer)
7-1. Using chemistry and materials science-based strategies to enhance cancer immunotherapy (Darrell Irvine)#
- intratumoral drug delivery inevitably becomes systemic
- idea: anchored immunotherapy (anchoring therapeutics to liposome larger than matrix pore size)
- still have limited lifespan of drug in tumor
Digression: kinetics of natural vs. synthetic immunizations#
- germinal center response = affinity maturation
- extended dosing allows for more kinds of B-cells to enter the germinal center, some of which may produce extremely good antibodies
- turning this into a real part of a vaccine
- alum has been traditionally viewed as a "depot-forming" adjuvant
- phosphorylated proteins bind very well to alum; add a phosphoserine "tag"
- Tyson Moyer
- antigen actually stays attached to alum, and now looks like a virus to the body
Apply vaccine work with alum to cancer immunotherapy#
- engineer a phosphoserine tag in the vector (add Fam20C expression vector as well for phosphorylation)
- Yash Agarwal
- AnkyraTx starting clinical trials
7-2. Human T-dependent B cell subsets in tissues and tumors (Shiv Pillai)#
- tumors are mostly cleared by CD8+ T-cells
B cells in context#
- lymphomas are most likely B cell lymphomas from the germinal center because the mutation rate is naturally so high in that location
Tumor antigens#
- tumor antigen needs to bind to MHC Class I (CD8+)
- antigens are often due to passenger mutations rather than driver mutations
- cancer needs to have many mutations to be immunogenic
Therapeutics#
- modalities
- small molecules
- i.e. enzyme inhibitors
- antibodies
- Ig-fusions
- Fc extends pharmacokinetics
- small molecules
B cells and cancer#
- more mutations = immunogenic (because more likelihood of tumor antigens to be produced)
- not set in stone yet; reviews will be equivocal
- B Lymphocytes and Cancer: A Love-Hate Relationship
Dai Fukumura, Role of Obesity and Exercise in Cancer#
- angiogenesis and adipogenesis form a vicious cycle
- obesity aggravates tumor desmoplasia in pancreatic cancers (increased fibrosis)
- leads to increased solid stress
- increased number of proliferating cells near adipocytes (why?)
- IL-6 overexpression by adipocytes
Yves Boucher, Reprogramming Pancreatic Cancer Tumor Microenvironment to Improve Therapy#
- PDAC tumor microenvironment
- highly fibrotic
- highly hypoxic
- immunosuppressive
- targeting/reprogramming tumor stroma
- hedgehog inhibition
- failed clinical trial; actually helped tumor progression
- PEGPH20 targeting of hyaluronan
- failed phase 3
- FAK inhibitors (reduces tumor fibrosis)
- failed clinical trial
- vitamin D analog (paracalcitrol)
- normalized CAFs; still in clinical trials
- Losartan (AT1 inhibitor)
- hedgehog inhibition
- alpha-SMA+ fibroblasts = myCAF
Lei Xu, Targeting the Tumor Microenvironment to Improve Tumor Control and Quality of Life#
- ovarian cancer (OvCa)
- vestibular schwannoma (acoustic neuroma) (NF2)
- lack of diagnostic tests for OvCa